Everything was falling into place for Cathleen Mattson. Recently married, armed with a master’s degree in neuroscience, she was planning to apply to medical school.
Then the unthinkable happened.
While running an errand with her mother, Mattson had a seizure that sent her to the hospital. The diagnosis: a brain tumor.
After an operation in 2003 and treatment with chemotherapy and radiation, Mattson’s remaining tumor is receding, but her life has been forever changed.
Complicated surgery on the tumor— located over the speech and motor area of the brain—severely affected Mattson’s ability to communicate. Although she may know what she wants to say, finding and uttering the words is now a struggle.
Fortunately, Mattson has found help at the UW’s Speech and Hearing Clinic, part of the Department of Speech and Hearing Sciences. She visits the clinic twice each week with her mother, Kay Rafferty. Slowly, steadily, she is regaining her language skills.

Mattson is in good company. About one thousand patients visit the Speech and Hearing Clinic each quarter, with communication concerns ranging from fluency problems (stuttering) to voice or articulation disorders to aphasia, an impairment of the ability to use or comprehend words, usually acquired as a result of a stroke or other brain injury.
“I feel so much gratitude that we found this program,” says Rafferty. “The focus here is one of discovery, figuring out what works for each individual. The knowledge and expertise of the staff is phenomenal.”
Good for Patients, Good for Students
While the Speech and Hearing Clinic has been invaluable for patients like Mattson, it plays another important role as a training facility for graduate students in speech and hearing sciences. The center’s treatment rooms sport one-way mirrors, with neighboring observation rooms for faculty, students, and patients’ families. Sessions are often recorded for later viewing and analysis by faculty and graduate students.
“When clients come in, we make it clear that while they will receive excellent service, they also will serve as a teaching tool for our students,” says Joan Hanson, clinic manager.
First- and second-year graduate students are the primary clinicians for treatment sessions. Faculty closely supervise the students’ work, observing at least 50 percent of the treatment sessions—twice the rate of supervision mandated by the American Speech and Hearing Association.
“Our faculty-graduate student ratio is very high,” say Nithya Siva, clinic instructor, who graduated from the program herself. “This is costly but important for the training of qualified therapists.”
Why would patients agree to be treated at a clinic where they are a “teaching tool” as well as a client? First, there’s the financial incentive. Treatment sessions cost “a fraction of what patients would pay on the outside,” says Hanson. But there are other benefits as well.

“I see the teaching environment as a big plus,” says Nellie Ohannes, who brings her two sons, ages 5 and 8, to the clinic for twice-weekly speech therapy. “The clinicians are always cheerful and well prepared. And the supervisors have been outstanding. They are so thorough and compassionate. It’s way more than just competence.”
Ted Paluchowski, who has been attending a support group for stroke survivors for six years, figures that he’s probably been through a generation of graduate students already. “I could probably do their homework for them,” he jokes. The students are a huge asset as facilitators, he says, because they “come with all that enthusiasm, all that positive energy.”
Finding Alternate Routes for Communication
Positive energy is essential when working with patients like Paluchowski and Mattson, who have suddenly lost the ability to communicate due to a stroke or other brain injury. The clinic regularly sees about 25 stroke survivors, in individual sessions and in two weekly support groups, each facing the wrenching prospect of a life altered by the loss of language skills.
“Language, communication, speech—all of this is incredibly complex work,” says Dr. Robert Miller, lecturer in speech and hearing sciences. “It is amazing that anyone can talk. More than any other motor activity, it happens so fast and requires so much precision. It is so easy for something to disrupt it, and so difficult to reestablish that.”
Mattson knows this only too well. After her brain tumor was removed, she had great difficulty finding the words needed to communicate. She was seen by language pathologists in the hospital, but her improvement was very slow. That all changed when she discovered the Speech and Hearing Clinic.
“This clinic tried different approaches until the lights started to come on,” says Rafferty, who observes each of her daughter’s sessions. “They take the time to see what works for each individual.”
One exercise that has helped Mattson involves repeating a handful of words over and over. In true Seattle fashion, the first words she chose to focus on were chair, coffee cup, and latte. “Once she had those words, other words started to come,” says Rafferty.
Miller explains that Mattson still has all the words in her head but needs help accessing them. “The dictionary is still there,” he says. “The difficulty is finding the word you want when you want it. It will never be as easy as before, but it will get easier to find the right word.”
In the meantime, one strategy is to work around the blockage, finding other ways to communicate. Rafferty likens it to finding alternate routes to avoid traffic. “It’s like I-5 is blocked each time you try to travel on it,” she says, describing her daughter’s language challenge. “The clinic has been working with Cathleen to find alternate routes to get where she needs to go rather than taking I-5.”
Sometimes these routes don’t involve speech. Patients are encouraged to use gestures, drawings, and sound effects to get their point across. Notebooks with cues—such as photos of family and friends, lists of children’s names, and career history—can also prove helpful. “The notebook is an augmentative tool, much like a wheelchair might be,” explains Nancy Alarcon, lecturer and director of the Speech and Hearing Clinic.
A Safe Place for Sharing
Alarcon runs two weekly support groups for aphasia patients. They gather around a table, armed with their notebooks, and talk about their lives. A graduate student facilitates the discussion, encouraging conversation through gentle but persistent probing. For some participants, sharing the simplest information is a challenge. But making the effort is a huge step in recovery, says Alarcon.
“It is so easy for people to sit back and stay quiet,” says Alarcon, “so part of what we do is draw them out with topics that are engaging.” In one recent session, the topic was the tsunami disaster. Patients also bring photos or other items from home to discuss with the group.
Paluchowski has been attending a support group for higher-functioning aphasia patients for nearly six years. He remembers how difficult the experience was at first.
“When I started, I had extreme difficulty speaking,” says Paluchowski, who had nearly completed a PhD at the UW before suffering a stroke in his 50s. “When I tried to talk, it was all a jumble. But Nancy [Alarcon] always forced us to make a presentation at each session, even though it might be very primitive. She had us keep pushing, pushing, pushing, and encouraged us to make our presentations longer. And there was a lot of encouragement from the others in the group.”
To hear Paluchowski today, his conversation flowing easily, it’s hard to grasp what he’s been through—and the challenges he still faces. “Oral comprehension is still difficult,” he admits. “In a room with too many people talking at one time, it’s very difficult. But I’ve gotten to the point where I have become relatively articulate, and I’m able to read and write again.”
Bob Anderson is in the same support group and shares Paluchowski’s gratitude. “It’s a place that feels safe,” he explains.
Anderson didn’t always feel that way. When he first joined, he found that his language skills were well above most of the other participants. “I was saying to myself, ‘These people are in worse shape than I am. What good is this to me?’” recalls Anderson. “I figured maybe I could help them. I felt very philanthropic. All of which was bull. It just took me a while to realize that the group was helpful to me, too. The other individuals provide a comfort and sharing that is very difficult to get elsewhere. A lot of people don’t understand the worth of that.”
Anderson now edits a newsletter for the clinic with stories by and about aphasia patients and their treatment. Although he often shares other individuals’ stories about their stroke and recovery, his own story has been elusive—buried somewhere in the portion of his brain affected by his stroke.
“I tell other people’s stories in the hope that by telling their stories, I can piece together parts of my own story,” he says, “and maybe trigger some memories.”
Keeping People in the “Game of Life”
For Anderson and Paluchowski—and countless others visiting the clinic—the emotional aspects of a communication disorder are nearly as challenging as the physical aspects. Recognizing and addressing this emotional component is an important part of students’ training in the clinic.
“Some of our clients have been very isolated, feeling like they are the only person who has ever had this experience,” says Alarcon. “They can feel very alone. Communication is so central to everyday life. Our goal is to keep people in the game of life.”
It’s not just the patients that need support. Their families and friends are also part of the equation. Spouses and children must adjust after a loved one has been affected by a language disorder. After a lifetime of communicating through talking, their relationship can be shaken when that is compromised.
“It’s a whole new situation for the family,” says Alarcon. “Sometimes we have one-on-one sessions with a spouse, or with a patient and spouse, to work on strategies for better communication. It’s intuitive to react to the spouse as you always have, but that’s often not effective. It’s just frustrating for everyone.”
Working with Kids
The emotional aspect is not limited to families affected by aphasia. Nellie Ohannes marvels at how the clinicians address family issues related to her sons’ language challenges.
“I have been so impressed by how they deal with the peripheral issues,” she says. “They have been very supportive of the total family environment. They see the total family context.”
Both of Ohannes’s sons were adopted from Russia. Eight-year-old Alex was born with a cleft lip and palate, severely affecting his speech. He has had four surgeries and has been visiting the clinic on and off since he was two.

“In the early days, a lot of the work was to help him find ways to communicate, because he was desperate to communicate,” says Ohannes. “He still loses a lot of air through his nose, which affects the sound of his speech, because his soft palate will not close all the way.” Exercises address the problem, including one in which he must use the sides of his tongue to direct air flow through a straw.
Younger brother John Samuel, age five, has experienced language delays that necessitated clinic visits as well. Each boy works with a clinician in a separate room while Ohannes watches from an observation room sandwiched between them.
For the graduate students who serve as clinicians, working with children presents its own set of joys and challenges. First, there’s the need to keep the child engaged—no small matter when you’re dealing with a pre-schooler. There can be behavior issues, or a lack of motivation. After all, it’s usually a parent rather than the child who makes the decision to visit the clinic.

Faculty supervision proves critical in such situations. Ohannes says that when the boys test their clinicians’ limits, the faculty member takes note of the situation and works with the student after the session to find a solution. She recalls one particularly difficult session, during which John Samuel crawled under a table and spent the hour hitting the floor and crying. “By the next session, the graduate student had all sorts of activities to do with him under the table,” she says with a laugh.
Sometimes faculty will help during a session if they sense that a student is struggling with a client’s behavior. “I’ve always appreciated that,” says Heidi Bigelow, a second-year graduate student. “And I like the opportunity to see a seasoned clinician come and work with the client a little bit.”

Leaving the Safety Net
By the time they earn their master’s degree, all speech-language pathology graduate students have worked with both children and adults on a wide range of issues, from aphasia to stuttering to voice concerns to language delays. Some work in schools after graduating; others head to hospitals or other health care facilities.
Bigelow, who has chosen a career in speech and hearing science because it combines her interests in English, science, children, and helping others, plans to work in a school setting. She is interning in the Mukilteo School District during her final quarter and finds the prospect of graduating bittersweet.
“I’m going to miss the clinic,” Bigelow admits. “It’s quite the safety net, with wonderful people to guide you. This is the ideal world—an amazing program with incredible people in it. It’s not going to be like that out there in the ‘real world.’”
Clients echo those sentiments. Cathleen Mattson, who was rarely able
to access any correct words just one year ago, perhaps says it best. “You guys are awesome,” she tells the clinic staff. “I feel like I’m getting much better. Because of you, I feel a change. It’s really . . it’s just the best.”
More Stories
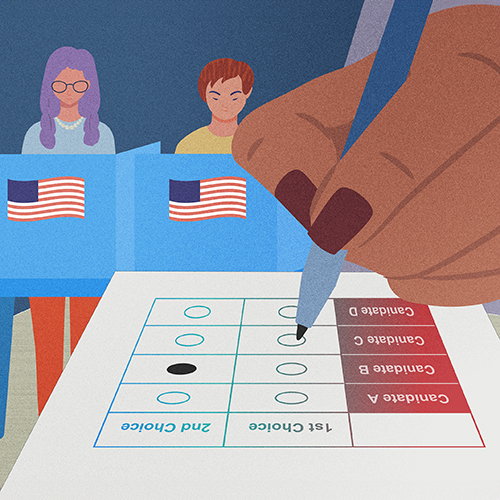
Democracy by the Numbers
Mathematics and Democracy, an undergraduate mathematics course, explores the role of math in many aspects of democracy, from elections to proportional representation.

A Statistician Weighs in on AI
Statistics professor Zaid Harchaoui, working at the intersection of statistics and computing, explores what AI models do well, where they fall short, and why.

The Mystery of Sugar — in Cellular Processes
Nick Riley's chemistry research aims to understand cellular processes involving sugars, which could one day lead to advances in treating a range of diseases.